|
If you are Breast Cancer Survivor and you would like to contribute your story to our Newsletter,
please send us a message here. |
Categories
All
Advocacy
Bone Health
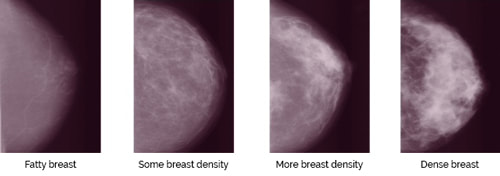
Breast Density
Breast Disease
Cancer Journey
Caregivers
COVID 19
COVID-19
Emotional Support
Environment
Exercise
Fatigue
Financial
Gender
Genetic Testing
Grief
High Risk
Hormone Replacement Therapy
Ignite
Implants
Intimacy After Cancer
LGBTQ
Lymphedema
Mammography
Masectomy
Meditation
Men
Mental Health
Metastasis
MRI
NBCC
Nutrition
Obesity
Pain
Pregnancy
Prevention
Radiation
Reconstruction
Reduce Risk
Rehabilitation
Screening
Sex
Side Effects
Sleep
Support
Support Groups
Surgery
Survivor
Survivorship
Treatment
Vaccine
Yoga
Young Women
Archives
January 2024
July 2023
April 2023
January 2023
October 2022
July 2022
April 2022
January 2022
October 2021
July 2021
April 2021
January 2021
October 2020
July 2020
April 2020
January 2020
October 2019
July 2019
April 2019
January 2019
October 2018
July 2018
April 2018
January 2018
October 2017
July 2017
April 2017
January 2017
October 2016
July 2016
April 2016
January 2016
October 2015
July 2015
April 2015
January 2015
October 2014
July 2014
April 2014
January 2014
October 2013
July 2013
April 2013
January 2013
October 2012
July 2012
April 2012
January 2012
October 2011
July 2011
April 2011
January 2011
October 2010
July 2010
April 2010
January 2010
October 2009
July 2009
April 2009
January 2009
October 2008
July 2008
April 2008
January 2008
October 2007
July 2007
April 2007
January 2007
October 2006
July 2006
April 2006
January 2006
October 2005
July 2005
April 2005
January 2005
October 2004
July 2004
April 2004
January 2004